
Introduction
The case of Lucy Letby, a nurse accused of murdering several infants, has captured national attention in the UK. The events surrounding her trial expose critical issues within the healthcare system, raising concerns over patient safety and the obligations of medical professionals. With the ongoing trial and testimonies from bereaved families, the implications of this case extend beyond the courtroom, compelling a reassessment of protocols in neonatal care.
Details of the Case
Lucy Letby, a neonatal nurse, was arrested in July 2018 after a series of unexplained infant deaths at the Countess of Chester Hospital between 2015 and 2016. Prosecutors allege that Letby intentionally caused the deaths or serious harm to at least 17 infants, including cases of insulin injections and air embolisms, leading to a high level of distress among families.
Evidence presented in court has included medical records, witness testimonies, and CCTV footage from the hospital, depicting troubling patterns coinciding with Letby’s shifts at the unit. The prosecution argues that Letby exhibited unusual behaviour, such as contacting the families of the deceased infants, which raised suspicions among her colleagues.
Despite the seriousness of the accusations, Letby has maintained her innocence, stating she was simply providing care to vulnerable infants. This dichotomy of perspectives not only highlights the complexities of the medical profession but also illustrates the devastating consequences for families affected by these tragic events.
Implications for Healthcare
The fallout from the ongoing trial will likely extend beyond individual accountability, bringing to light systemic issues within hospital management and oversight. The case prompts essential discussions about the need for vigilant reporting systems, proper staffing, and mental health support for healthcare professionals working in high-stress environments.
Families have begun to vocalise their concerns, demanding better accountability and transparency from medical institutions. Campaigns for reform have emerged, advocating for improved protocols to protect vulnerable patients, especially in neonatal care.
Conclusion
The Lucy Letby case serves as a tragic reminder of the vulnerabilities present within healthcare systems. As the trial unfolds, the outcomes will likely inspire substantial discussions around patient safety, ethics in medical practice, and the profound trust placed in healthcare providers. For the families affected, closure may be years away, but their courage in seeking justice could ultimately drive essential change within the UK’s healthcare framework.
You may also like

The Role of Face Masks in Public Health Today
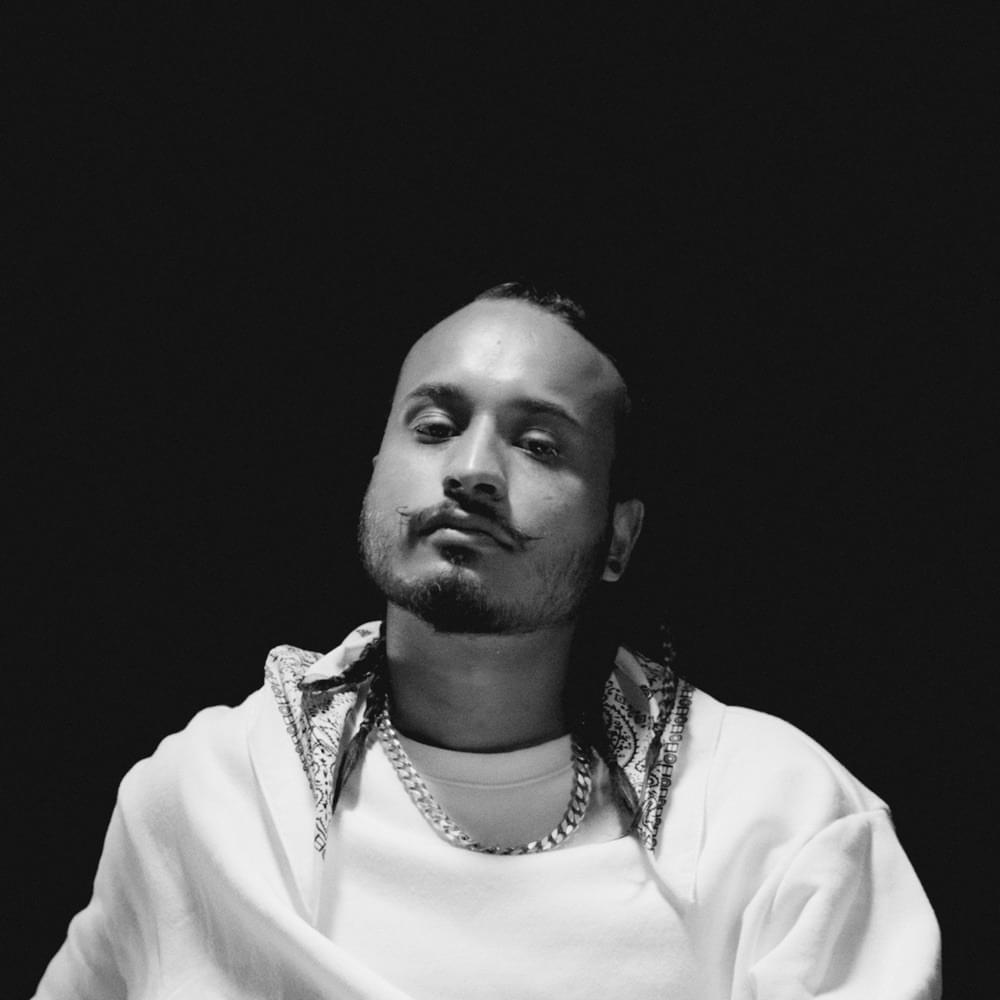
The Life and Crimes of Rehman Dakait
